Abstract
Introduction: Although infections are a leading cause of morbidity and mortality in MDS patients, there is limited evidence on causative organisms and resistance patterns in this patient population. This study, the largest series of infection in MDS patients, seeks to comprehensively analyse infection in this cohort.
Method: CT scan, microbiology results and hospital admission ICD codes from January 1999 to April 2017 were analysed for 657 MDS patients enrolled in the South Australian MDS (SA-MDS) registry. Cox regression analysis was performed to ascertain risk factors for developing infection.
Results: There were 531 primary and 126 therapy-related myeloid neoplasm (t-MN) patients with median age of 69.2 (18-97) years. According to Revised International Prognostic Scoring System (IPSS-R), 44.7% of patients were classified as Intermediate, High and Very High risk. The majority of the cohort (377/657; 57.3%) received best supportive care and 265 had disease modifying therapy including azacitidine (n=142), chemotherapy (n=74) and stem cell transplantation (SCT) (n=25).
There were 2450 hospital admissions and 1312(53.5%) were infection-related, in 464/657 patients. The most common sites of infection were lower respiratory tract infections (LRTI) n=449(33.2%), fever with no known source n=356(26.3%) and skin and soft tissue (SSTI; 235, 17.3%).
During the study period, 1613/16176 (10%) of microbiology tests were positive. The most common positive tests were blood cultures (494, 30.6%), respiratory viral PCR (227, 14.0%) and bacteriology (other sites; 216, 13.4%).
The most common isolates were bacteria (67.3%) followed by viruses (28.1%) and fungi (4.6%). The most common bacteria were gram negative bacilli (GNB); E. coli n=81(12%), Pseudomonas spp. n=64(9%) and Klebsiella spp. n=56(8%), and the most common gram-positive isolates were Staphylococcus aureus n=114(20%) and Enterococcus spp. (37, 7%).
There were 192 episodes of bacteraemia in 179 patients. The most common causative organisms were E. coli n=32(16.7%), Klebsiella spp. n=18(9.4%) Pseudomonas spp. n=25(13%), coagulase negative staphylococci n=26(14%), Streptococcus spp. n=22(11%) and Enterococcus spp. n=14(11%). The proportion of GNB bacteremias significantly increased over time (45.8% 1999-2005; 40.0% 2006-2011 and 59.4% 2012-2017 [p=.004]) without increased resistance to commonly used antibiotics. There were 21 enterococcal bacteremias with significant increase in proportion of vancomycin resistant Enterococcus (VRE) after 2011 (p<0.001).
The most commonly isolated respiratory viruses were rhinovirus (98, 43.2%), influenza (34, 15%) and parainfluenza (34, 15%), Cytomegalovirus was identified in 154 specimens from 31 patients, all following SCT.
70 patients had probable or confirmed fungal infection, with 52 (74.3%) patients having positive fungal cultures or CT findings. The most common sites of fungal infection were chest n=21(76.9%), followed by skin n=5(9.6%), urine n=4(7.7%) and blood n=3(5.8%). Aspergillus n=17(44.7%) was most commonly isolated, followed by Candida spp. n=15(39.5%) and Rhizopus n=3(7.9%).
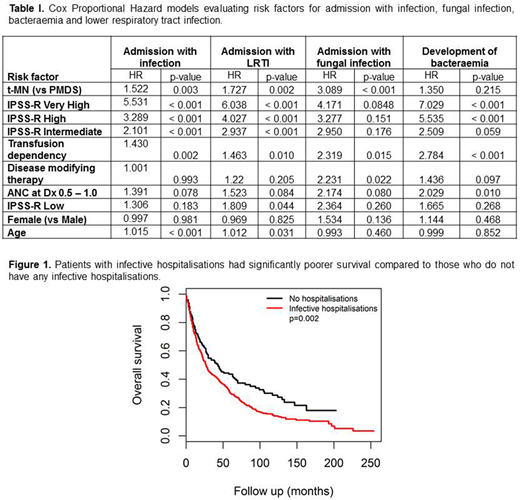
We performed a Cox regression analysis of the risk factors for development of infection requiring hospitalisation, specifically with LRTI, fungal infection and bacteraemia (Table I). Significant predictors were increased age, t-MN, higher IPSS-R score and being transfusion dependent at diagnosis. Receiving disease modifying therapy was a significant risk factor for hospitalisation with fungal infection (p=0.022).
Additionally, patients who had hospitalisations for infections had poorer overall survival compared to hospitalised patients without infection (p=0.002, Figure 1).
Conclusions: Greater than 50% of hospital admissions in MDS patients were complicated by infection and this was associated with a significant reduction in survival. The most common sites were LRTI, followed by bacteraemia and SSTI.
Bacteraemia from GNBs increased over the study period without significant change in resistance patterns, while prevalence of VRE increased since 2011. Respiratory viruses, including influenza, caused significant morbidity, suggesting a role for routine vaccination.
RBC transfusion dependency, t-MN and disease modifying therapy are independent risk factors for fungal disease. This highlights a cohort of patients that would benefit from anti-fungal prophylaxis.
Hiwase:Celgene: Research Funding; Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal